“Walking on clouds” may sound like a great way to spend a particularly boring meeting – but when it becomes your everyday reality, it is anything but pleasant. Also known as “floppy toes” or “flail toes,” floating toe syndrome is a common small toe deformity. Although rarely as painful as bunions or big toe problems, it can still do a number on your posture, balance, and general well-being.
What is a floating toe?
Floating toes happen when any of your toes are permanently lifted off the ground, even when you stand in a neutral position. It can develop on any of your lesser toes, but it is most common on the second toe.

How bad is a floating toe?
When we walk, our toes are supposed to stay in contact with the ground for about 75% of the time. This helps them distribute the load evenly across your foot plate, push your body upwards, and stabilize your spine and joints.
If one of your toes is sticking in the air during this process, the damage may not be radical or even evident – at first. However, you’ll find it harder to walk or run due to poor biomechanics — essentially, if you’re short a toe on one side, your body will compensate some other way.
One of the first complications is chronic metatarsalgia or pain in the ball of the foot. You may find it harder to keep your balance and you will subconsciously adjust your walking speed or stride length to accommodate the pain. After years of malalignment, all these small posture adjustments will also increase the wear and tear on your other weight-bearing joints.
So, if you have a floating toe today, you may not notice anything beyond extra joint stiffness after a hard day. But in the long term, the damage can be extensive and lead to more serious toe deformities.
What causes floating toe?
Floating toes may develop because:
- Your metatarsals (the small bones in your toes) are lifted upwards.
- The extensor tendons or ligaments under the bones are too tight or too long.
- Your toe joints are being “pulled“ or “pushed” by a big toe misalignment.
- There is some other issue restricting the range of motion of your big toe (hallux limitus).
- The metatarsophalangeal joint (MTP Joint) is too stiff or compressed by the other toes.
If that all sounds tremendously complicated, just keep one thing in mind: feet are like a very delicate house of cards. Sure, we jump and run and kick with them — but any dysfunction in the foot and ankle area will eventually cause something else to suffer.
The same thing happens with floating toes. Many other foot deformities can trigger a floating toe, which in turn, will make other posture and alignment problems worse. Let’s take a look at some of the most common causes of floating toe syndrome.
Bunions and hammertoe
Bunions (hallux valgus) are part of the bread and butter for any podiatrist. They are “bony bumps” that form on the outer side of the big toe joint, as the joint progressively moves out of place.
Severe bunions, in turn, can lead to a hammertoe: when the middle joint of any of the lesser toes starts to bend out of place. When left untreated, the “bent” joint will become stiff and fixed, and it may permanently leave the affected toe floating.
The process doesn’t stop there; once you develop a floating second toe, the risk of a hammertoe on the third or fourth toes will increase. This will also increase the overall discomfort of the original bunion.
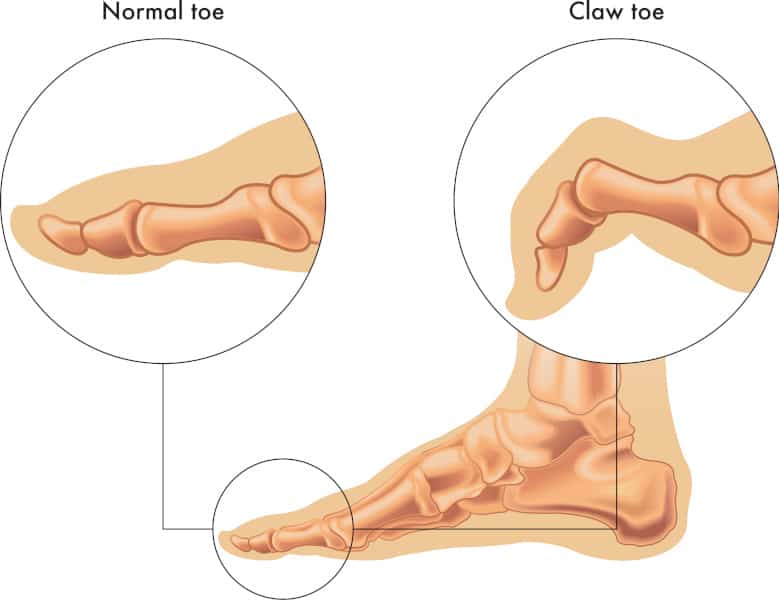
Claw toes
So-called “claw toes” are considered a “lesser deformity,” as they don’t affect your balance as much as a full-blown floating toe. Instead, claw toes happen when the proximal interphalangeal joint (the one between the first and second toe bones) begins to curve upwards. This makes it look a bit like a bear’s claw.
You’ll note that we almost always talk about claw toes in the plural, as they rarely affect just one toe. If left to progress, claw toes can lead to a floating toe. If the proximal phalanx in the second toe curves too high, it will leave the tip of the toe hanging. In addition, having a floating second toe will make it more likely for the third, fourth, and fifth toes to curl into claws.
Floating toe after surgery
Hammertoes themselves can put you on the path toward a floating toe. However, sometimes the remedy’s also the cause – or in this case, surgeries such as a Weil osteotomy, joint resection, or arthrodesis can lead to a floating toe.
Weil osteotomies are among the most common foot surgeries in the realm of podiatry. They are usually remarkably safe – but complications do happen. The surgery itself is designed to slightly shorten one of the metatarsals, which will prevent it from “bending” into a hammertoe.
However, during hammertoe surgery, surgeons may shorten the flexor ligament or the bone a bit too much. The resulting toe will be too short to touch the floor and lead to a floating toe.
Floating toe and plantar plate injury
The plantar plate is a tough layer of cartilage on the soles of your feet that holds the toes and foot together. When this plate tears, either due to an accident or a severe sprain, it will tense up and pull all the muscles, ligaments, and tendons it is attached to. This will, in turn, pull the toes upward, and create a floating toe.
Can a floating toe be corrected?
There are two ways to treat a floating toe: we can fix it with surgery, or we can manage it with less invasive techniques. Neither is absolutely better than the other: the right choice will depend on the extent of the problem, which other issues it’s causing, and whether you have any other toe deformities.
Surgical correction for floating toes
“Fixing with surgery” often sounds like a straightforward solution. When it comes to floating toes, the answer is rarely that simple. To repair a floating toe, we need to add some extra length (even a few millimeters) to your toes. This is usually done with a “flexor to extensor” transfer. In extreme cases, we can also use bone grafting to lengthen the extensor ligaments. This should keep it from being “pulled back.”
Either way, we are talking about a much more high-tech and delicate procedure than shortening the metatarsal bone or fusing two joints together. If you’ve already had surgery on that toe, the existing scar tissue will create an extra hurdle: the more we poke around soft tissue, the higher the chance that it won’t end up as it should.
The surgery gets remarkably more complex if more than one toe is affected.
Floating toe management
Non-invasive management remains the go-to option for floating toes. A combination of taping and physical therapy can pull the toe back to the ground.
If you are looking for a slightly more sophisticated treatment option, custom orthotics, or “bracing socks” can also help manage floating toes, and will keep them from progressing. Overall, results from these conservative strategies are much more predictable, if less fancy, than surgery.
Need floating toe correction near L.A.? UFAI is your best bet
Led by a team of board-certified DPMs (Doctors in Podiatric Medicine), UFAI is one of SoCal’s leading centers for the holistic treatment, management, and prevention of foot and ankle issues.
Our physicians and supporting staff all specialize exclusively in the foot. We understand the delicate connections between dorsal pain, a small fracture in the metatarsal head, or a bunion – and we know how it can impact your overall health. Whether you are requesting a surgical consultation, or need to follow-up on a recurring problem, we will make sure to deal with all angles of your problem.
To schedule a consultation with one of our renowned podiatrists and bunion surgeons, please call (855) 872-5249 or make an appointment now.
University Foot and Ankle Institute is conveniently located throughout Southern California with podiatry clinics in (or near) Santa Monica (on Wilshire Blvd.), Los Angeles, Beverly Hills, West Los Angeles, Sherman Oaks, and the San Fernando Valley, Manhattan Beach, and the South Bay, LAX, Westlake Village, Valencia, Santa Clarita, and Santa Barbara.
- Avoiding Foot and Ankle Overuse Injuries While Dog Walking - July 17, 2023
- What is Floating Toe Syndrome? - June 12, 2023
- Is there a link between gout and heart disease? Studies Say Yes - February 22, 2022
Leave a Reply