According to the Centers for Disease Control, diabetes (specifically diabetes mellitus) affects over 34 million Americans. The associated elevated blood sugar levels can cause diabetic patients two serious problems: nerve damage (neuropathy) and poor circulation.
These problems lead to further health complications, especially in the feet. In this post, we’ll be focusing on Charcot foot.
What is Charcot Foot Syndrome?
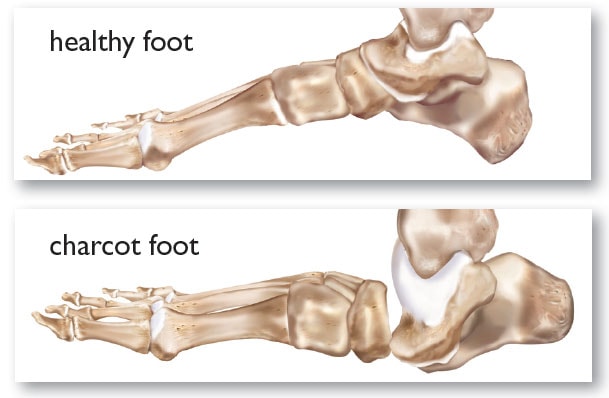
Charcot foot is a consequence of peripheral neuropathy (damage to the nerves in the lower legs and feet). According to an article published in Diabetes Care, diabetic neuropathy has become the most common cause of Charcot foot.
Because of the nerve damage, diabetes patients can suffer injury to the foot but not feel the associated pain. A sore, infection, sprain, or broken bone that goes untreated because the patient doesn’t notice it can continue to worsen, resulting in Charcot foot.
Charcot is considered an inflammatory condition that affects the bone and soft tissue of the foot and ankle. Charcot neuroarthropathy (neuroarthropathy being a joint disorder caused by loss of feeling) is a progressive condition that weakens foot bones. The weakened bones are prone to breaks or dislocation and, if not addressed in time, the patient can suffer joint dislocation or collapse, leading to foot deformity.
Dr. Baravarian discusses Charcot foot
Why is Charcot foot dangerous?
As mentioned, untreated diabetic Charcot foot can cause the joints of the foot to collapse. This severe deformity can result in long-term disability. An advanced complication is Charcot midfoot collapse (also known as “rocker-bottom foot”). The bones and joints in the middle of the foot drop lower than the forefoot and hindfoot giving the foot a “rocker”-like shape. The rocker-bottom deformity is a series consequence of Charcot foot. With appropriate early treatment, this complete collapse can be avoided.
Charcot deformity can also cause pressure sores or ulceration. Untreated, the weakening of the bones and joints can also lead to hammertoes and ankle instability.
Without proper treatment, the deformity can lead to bone infection (osteomyelitis) and, in severe cases, amputation.
What are the symptoms of Charcot Foot?
Despite potentially resulting in severe deformity, patients with Charcot foot don’t generally experience pain. This is because diabetic Charcot foot is generally accompanied by peripheral neuropathy. Nerve damage in the foot dulls or eliminates the sensation of pain.
The most obvious symptoms of Charcot foot are swelling of the affected foot (that isn’t caused by injury or foot ulcer), redness of the skin, and increased skin temperature.
Charcot Foot Diagnosis
Acute Charcot neuroarthropathy can sometimes be tricky to diagnose. X-ray images may not reveal anything or may be confused with different foot problems. For early and accurate diagnosis of Charcot foot, see a trained foot specialist (podiatrist) or a doctor who’s familiar with diabetes treatment.
Magnetic resonance imaging (MRI) allows the detection of subtle changes in the bone that X-rays might miss.
Radiographic evidence of Charcot foot includes subluxation (slight dislocation) of the joint, bone fragmentation, and bone mineralization.
Treatment for Charcot Foot
The key goals of early-stage Charcot foot treatment are: immobilization and non-weight bearing of the foot, treat bone disease (usually with a cast, sometimes with bisphosphonates and other supplements), and prevent new fractures.
Nonsurgical Charcot Foot Treatment
There are a few options for non-surgical treatment. With early diagnosis, the diabetic Charcot foot can be addressed in its early stages.
Casting
Securing the affected foot and ankle with a total contact cast or boot can be effective for treating early Charcot foot syndrome. This protects the bones and reduces swelling. The total contact cast technique is used to heal diabetic foot ulcers and protects neuropathic patients’ feet during the early stages of Charcot.In addition, the patient will have to keep weight off the foot (also called “offloading”) while the bones heal. Crutches, a knee-walker, or a wheelchair may be necessary.
The doctor may use a special brace (orthosis) to correct and compensate for the bone deformity. Read more about Charcot foot braces here.
Custom Shoes for Charcot Foot
When the swelling has been reduced and the bones are fusing back together, you may need a custom walking boot or orthopedic shoes. Due to the poor blood flow in the feet, injuries and sores are slow to heal in diabetic patients. Regular, over-the-counter shoes don’t properly fit feet with Charcot deformities, potentially leading to scrapes, sores, and infections.
A common device for patients recovering from acute Charcot foot is Charcot Resistant Orthotic Walker (CROW). This sturdy shoe protects the whole foot while still allowing normal walking.
Charcot Foot Surgery
If the Charcot deformity puts the patient at higher risk for ulcers, or if protective footwear has not been effective, surgery may be recommended. For severe deformity or joint looseness, surgery may be required for appropriate realignment.
Fractures in the softer bones of diabetics are typically more complex. For this reason, surgery usually involves more hardware (plates and screws) than would be required in non-diabetics.
The specifics of surgery will depend on the primary problem.
Heel Tightness
A mild deformity with tightness at the back of the heel. Diabetic foot ulcers in the forefoot that don’t respond to casting or protective footwear can often be treated with Achilles tendon lengthening.
Lengthening the Achilles tendon reduces pressure on the midfoot and forefoot. This gives the ulcer time to heal and lowers the chances of it returning.
Bony Prominences
A severe deformity may result in plantar prominences (bony bumps on the bottom of the foot). Again, if not responsive to shoe modification, it will require surgery. If the deformity is stable, the bony prominence can be surgically shaved off.
If the bones are loose at the site of the prominence, the deformity is considered “unstable.” In this instance, the bones will require repositioning and arthrodesis (joint fusion).
Ankle Deformity
Charcot joint in the ankle is hard to treat with only a brace. Generally, fusion of the ankle and the joint below the ankle are required to hold the foot straight. Unfortunately, due to the poor quality of the bone and soft tissue, there is a high risk of infection or of the bone not healing.
If the fusion doesn’t heal or becomes infected, amputation may be necessary.
Diabetic Charcot Foot Prevention
The best treatment for diabetic foot conditions is prevention.

About 90-95% of Americans with diabetes have Type 2 diabetes, which can be prevented or delayed through diet and exercise. If you’re at risk for diabetes, work with your doctor to monitor your blood sugar levels.
If you have diabetes (and especially if you have diabetic peripheral neuropathy), carefully inspect your feet every day. The nerve damage inhibits your ability to feel pain, so check every day for injuries, sores, redness, swelling, or other changes.
Other steps to protect your feet include:
- Keeping blood sugar levels under control. As Charcot foot is a complication of diabetes, regulating blood sugar levels can help reduce the progression of nerve damage.
- Having regular foot exams and checkups with your foot and ankle surgeon.
- Avoiding injury to the feet. For example, avoid bumping the foot or over-exercising.
- Wearing comfortable shoes with a roomy toe box.
- Following surgeon’s instructions for long-term treatment to prevent further complications
Why choose University Foot and Ankle Institute for your Diabetic Foot Care?
Whether you’re already struggling with Charcot foot or just want advice on caring for your diabetic feet, our nationally recognized foot and ankle doctors offer the most advanced foot care and the highest success rates in the nation. We are leaders in the research and treatment of all foot and ankle conditions.
At University Foot and Ankle Institute, we take our patients’ safety seriously. Our facility’s Covid-19 patient safety procedures exceed all CDC recommendations. Masks are required in our institutes at all times.
For more information or to schedule a consultation, please call (877) 736-6001 or make an appointment now.
We are conveniently located through the Los Angeles area with locations in or near Santa Monica (on Wilshire Blvd.), Beverly Hills, West Los Angeles, Manhattan Beach, Northridge, Downtown Los Angeles, Westlake Village, Granada Hills, and Valencia, California.
- Flip-flops Causing You Pain? Protect Your Feet This Summer! - April 23, 2024
- 9 Running Tips from Sports Medicine Experts - November 8, 2023
- Common Foot Problems In Aging Feet: What To Watch Out For - October 16, 2023
Leave a Reply