
Our ankles are overused and underappreciated. They are constantly called upon to bear multiples of our body weight (150% when we walk, 800% when we run).
Ordinary daily activity requires our ankles to constantly swivel and flex in three dimensions, like a piece of smooth-running machinery.
But sometimes the ankle machinery misbehaves, it suddenly refuses to swivel. Then the next moment, that same ankle is suddenly unstable. First there is gravel in the gears, and then there are no gears at all.
The leg bone’s connected to the ankle bone
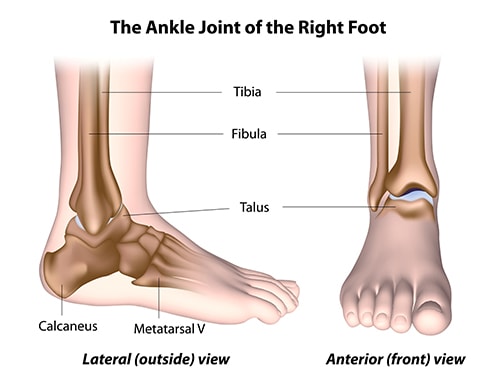
The juncture between the talus bone (ankle) and the tibia (leg bone) enables our ankles’ ability to smoothly swivel. The tibia is the larger of the two bones that run from the knee to the ankle. The talus is the big lump of bone that is the most prominent component of the ankle. The function of the talus is to transfer weight-bearing from the bones of the shin to the foot.
When your ankle catches, or suddenly feels unstable, the culprit is most likely a “talar osteochondral lesion.” (To break that down: “osteo” refers to bone, “chondral” relates to cartilage, and “lesion” means wound.)
The top of the talus is shaped like a dome, and the lower end of the tibia rests on that talar dome.
Both the talus’ dome and the end of the tibia are coated with an extremely durable and slick substance known as cartilage. The layers of cartilage on the tibia and talar dome are each between 1/8-inch and 1/4-inch thick.
This coating of articular cartilage is extremely tough and yet very smooth. It is meant to provide a lifetime of friction-free interaction between the tibia and the talus.
But sometimes trauma, either sudden and forceful or repetitive over time, can disrupt the harmonious relationship between the tibia and the talar dome.
So why does my ankle feel like it’s catching?
Your ankle may be locking up due to an osteochondral lesion.
An osteochondral lesion of the ankle occurs when trauma knocks loose a chip of bone or fragment of cartilage. That piece then catches between the tibia and the talus.
That feeling of gravel in the gears occurs when the chip of loose bone or cartilage fragment prevents the tibia from smoothly sliding over the talus.
The vacancy where the bone chip or cartilage fragment used to be creates the sudden feeling of ankle instability. Untreated, this cartilage damage can develop into cysts.
Because they usually start with trauma, osteochondral injuries are most likely to occur in the younger and more athletic population.
What else could cause my ankle to lock up?
Osteochondritis dissecans (essentially, lack of blood supply) can prime your ankle for osteochondral lesions of the talus.
The intersection between the talus and the tibia doesn’t have as bountiful a supply of blood as other joints. When a diminution of blood flow causes the talar cartilage to dry out, it results in the condition known as osteochondritis dissecans (OCD).
Whether the cause is insufficient blood flow, the sudden trauma typical of severe ankle sprains, or micro-fractures caused by repetitive stress, the resulting talar dome lesions can be painful, debilitating, or even disabling.
What are the symptoms of talar osteochondral lesions?
In addition to the feeling that a dislodged fragment has caused the ankle to lock up, the symptoms of an osteochondral lesion include:
- prolonged ankle pain
- swelling
- general instability of the ankle joint
After the type of trauma that causes an ankle sprain, the initial pain and swelling should decrease with appropriate attention. So, pain that persists for months, despite appropriate treatment, may justify concern for an osteochondral lesion.
How are talar osteochondral lesions diagnosed?
The diagnostic process begins with the taking of an injury history, followed by a physical examination. This examination will include evaluation of local tenderness and swelling and assess range of motion.
Because osteochondral lesions are frequently accompanied by injury to ligaments, joint instability should also be measured.
X-rays are useful for diagnosis, and an MRI or CT scan is frequently necessary to fully evaluate the extent of the injury.
What are the options for treatment of osteochondral lesions of the talus?
For most osteochondral injuries, the initial treatment plan will be conservative. The joint will be immobilized, with no weight-bearing, for several weeks with periodic follow-ups.
Nonsteroidal anti-inflammatory drugs can help with the pain and swelling. After the immobilization period, physical therapy can begin to gradually increase range of motion and weight-bearing activity.
When non-surgical treatment is unsuccessful, surgical intervention is effective
As is the case with nearly all surgical interventions, osteochondral lesion surgery begins with the removal of dead, dying, and decayed material (debridement). This leaves only healthy bone and tissue.
Arthroscopy and bone transplantation
Arthroscopic surgical techniques are the optimal mode of surgical treatment for osteochondral injuries. These techniques insert tiny cameras and minuscule surgical instruments, which enable both direct visual evaluation and repair.
Bone marrow stimulation, by means of intentionally induced microfractures, has also demonstrated an impressive success rate in the re-creation of healthy cartilage.
When the lesion is large or involves subchondral bone that’s deep below the damaged cartilage, bone and cartilage can be transplanted into the injured region. The transplanted bone and cartilage can come either from elsewhere in the patient’s body (autograft) or from a donor or a cadaver (allograft).A revolutionary new product called BioCartilage results in a stronger ankle joint, faster recovery, and a reduced chance of reinjury than traditional methods.
Because the talus’ dome lacks a strong blood supply, healing a damaged talus can take longer than most other bones.
Patients recovering from a severely damaged talus may be facing the use of crutches for a period of months. Afterward, they will likely wear a walking boot for a significant period of time.
Why choose University Foot and Ankle Institute for your foot ankle treatment options?
If you are experiencing foot or ankle pain, we’re always here to help. At UFAI, our mission is to provide the best available treatment techniques. We want our patients to be pain-free and back to their daily activities as soon as possible.
Our nationally recognized, board-certified Doctors of Podiatric Medicine (DPMs) and foot and ankle surgeons offer the most advanced care, the highest success rates in the nation and are leaders in developing surgical technologies that improve every patients’ outcome.
We realize our patients lead busy lives. That’s why our podiatry clinics include their own digital x-ray machines as well as in-house or very conveniently located MRIs and CAT scanners. Local access to this equipment facilitates prompt diagnosis with minimal inconvenience.
Additionally, several of our clinics have in-house physical therapy facilities, giving (1) our therapists immediate access to our doctors and (2) our doctors the ability to closely monitor their patients’ therapeutic progress.
For more information, or to schedule a consultation, please call (877) 736-6001 or make an appointment online now.
At UFAI, we take our patients’ safety seriously. Our clinics’ and surgery centers’ Covid-19 patient safety procedures exceed all CDC recommendations during this pandemic. Masks are required in our institutes at all times.
We are conveniently located throughout Southern California and the Los Angeles area. Our doctors are available at locations in or near: Santa Monica, Beverly Hills, West Los Angeles, Manhattan Beach, Northridge, Downtown Los Angeles, Westlake Village, Granada Hills, and Valencia, California.
- What To Do When Your Toenail Is Falling Off - October 21, 2024
- How To Tell If You Have Wide Feet - October 3, 2024
- 15 Summer Foot Care Tips to Put Your Best Feet Forward - July 1, 2024
Leave a Reply