- Home
- Foot & Ankle Conditions
- Less Common Conditions
- Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome: causes, symptoms and treatment
- Published 11/1/2023
- Last Reviewed 6/11/2024
What's tarsal tunnel syndrome?
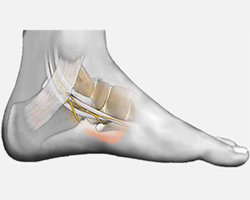
The tarsal tunnel is located inside of the ankle. Running next to the ankle bones, this narrow tunnel is a path for many of the foot and ankle’s tendons, nerves, and blood vessels. It protects many important structures, such as the posterior tibial nerve, and maintains foot strength, flexibility, and health.
Tarsal tunnel syndrome (TTS) is a disorder caused by trauma to the tibial nerve (or its branches). Similar to carpal tunnel syndrome of the wrist, it is usually due to compression or entrapment of the nerve as it passes through the tarsal tunnel.
- Previous
- Condition
-
Foot and Ankle Surgeon at University Foot and Ankle Institute
Dr. Abimbola Johnson completed his undergraduate degree at Loyola University Chicago, where he played Division II rugby and was also involved in social justice clubs aimed at helping younger students prepare for college.
Upon graduation, he entered Scholl College of Podiatric Medicine, where he served as president of the practice management club and volunteered as coordinator at the Free Foot Clinic in Chicago. He served his residency at Regions Hospital/Health Partners in St. Paul.
Dr. Johnson provides comprehensive medical and surgical care for a wide spectrum of foot and ankle conditions, including common and complex disorders and injuries. The doctor is uniquely qualified to detect the early stages of disease that exhibit warning signs in the lower extremities, such as diabetes, arthritis, and cardiovascular disease.
Dr. Johnson can be seen at our Santa Barbara location
 I’ve been so happy with the expertise, patient care, and recovery so far. I have one more surgery to go and am really hopeful t...Emily C.
I’ve been so happy with the expertise, patient care, and recovery so far. I have one more surgery to go and am really hopeful t...Emily C. The doctor and staff always provides excellent treatment and service.Dorothy W.
The doctor and staff always provides excellent treatment and service.Dorothy W. Suzanne at UF&AI saved my Ironman! I started to develop ankle stiffness about two weeks before my first Ironman. I was referr...Robert U.
Suzanne at UF&AI saved my Ironman! I started to develop ankle stiffness about two weeks before my first Ironman. I was referr...Robert U. SO HAPPY TO FINALLY FIND A DOCTOR AND ASST I FEEL COMFORTABLE WITH !! I WAS VERY PLEASED WITH THE DR GINA AND HER MALE ASST T...Marguerite S.
SO HAPPY TO FINALLY FIND A DOCTOR AND ASST I FEEL COMFORTABLE WITH !! I WAS VERY PLEASED WITH THE DR GINA AND HER MALE ASST T...Marguerite S. They really try hard to make me feel complete and on point.Lester S.
They really try hard to make me feel complete and on point.Lester S. The doctor was very thorough and caring.Erika F.
The doctor was very thorough and caring.Erika F. Excellent job. Have a Merry Christmas and a Happy New YearValerie S.
Excellent job. Have a Merry Christmas and a Happy New YearValerie S. Office and examination rooms are very clean and comfortable. Staff are very professional and friendly.Myrna M.
Office and examination rooms are very clean and comfortable. Staff are very professional and friendly.Myrna M. I have horrible feet. Bad DNA. My aunt and my mother have both had multiple surgeries. I had hallux rigidis in both feet and ne...Citizen L.
I have horrible feet. Bad DNA. My aunt and my mother have both had multiple surgeries. I had hallux rigidis in both feet and ne...Citizen L. I have been to other locations and it was ok. The staff at the Westlake Village location is exceptional.Lynne B.
I have been to other locations and it was ok. The staff at the Westlake Village location is exceptional.Lynne B. Appointments always went smoothlyArthur H.
Appointments always went smoothlyArthur H. Great serviceDavid K.
Great serviceDavid K.
-
 Listen Now
Swollen Feet During Pregnancy
Read More
Listen Now
Swollen Feet During Pregnancy
Read More
-
 Listen Now
Bunion Surgery for Athletes: Can We Make It Less Disruptive?
Read More
Listen Now
Bunion Surgery for Athletes: Can We Make It Less Disruptive?
Read More
-
 Listen Now
Non-Surgical Treatment for Plantar Fasciitis – What Are Your Options?
Read More
Listen Now
Non-Surgical Treatment for Plantar Fasciitis – What Are Your Options?
Read More
-
 Listen Now
Could Feet Be the Windows to Your Health?
Read More
Listen Now
Could Feet Be the Windows to Your Health?
Read More
-
 Listen Now
Should I See a Podiatrist or Orthopedist for Foot Pain and Ankle Problems?
Read More
Listen Now
Should I See a Podiatrist or Orthopedist for Foot Pain and Ankle Problems?
Read More
-
 Listen Now
How To Tell If You Have Wide Feet
Read More
Listen Now
How To Tell If You Have Wide Feet
Read More
-
 Listen Now
Do Blood Pressure Medicines Cause Foot Pain?
Read More
Listen Now
Do Blood Pressure Medicines Cause Foot Pain?
Read More
-
 Listen Now
What To Do When Your Toenail Is Falling Off
Read More
Listen Now
What To Do When Your Toenail Is Falling Off
Read More
-
 Listen Now
What Is Erythromelalgia?
Read More
Listen Now
What Is Erythromelalgia?
Read More
-
 Listen Now
Bunion Surgery for Seniors: What You Need to Know
Read More
Listen Now
Bunion Surgery for Seniors: What You Need to Know
Read More
-
 Listen Now
Moore Balance Brace: Enhance Stability and Prevent Falls for Better Mobility
Read More
Listen Now
Moore Balance Brace: Enhance Stability and Prevent Falls for Better Mobility
Read More
-
 Listen Now
Pediatric Bunion Surgery
Read More
Listen Now
Pediatric Bunion Surgery
Read More
-
 Listen Now
How Many Steps Do I Need A Day?
Read More
Listen Now
How Many Steps Do I Need A Day?
Read More
-
 Listen Now
15 Summer Foot Care Tips to Put Your Best Feet Forward
Read More
Listen Now
15 Summer Foot Care Tips to Put Your Best Feet Forward
Read More
-
 Listen Now
What Are Shin Splints?
Read More
Listen Now
What Are Shin Splints?
Read More